.97077bf4.webp&w=640&q=75)
Unraveling Multiple Sclerosis: A Comprehensive Guide

Multiple sclerosis (MS) is a complex neurological disorder that affects millions of people worldwide. In this article, we will dive into the intricate world of MS, exploring its causes, symptoms, and treatments. Our aim is to provide you with a clear understanding of this condition and address some of the most frequently asked questions.
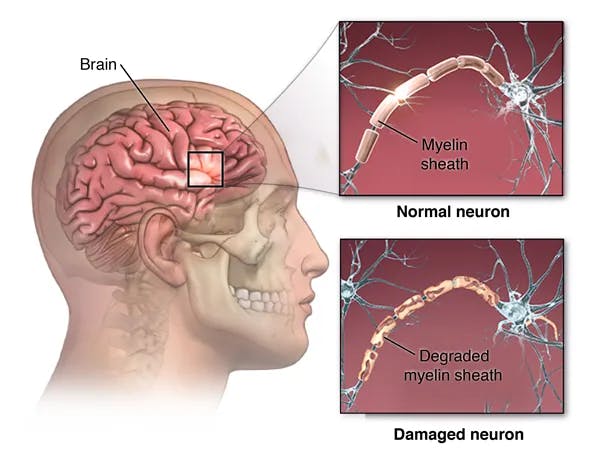
What is Multiple Sclerosis?

Multiple sclerosis is a chronic autoimmune disorder that affects the central nervous system (CNS), which comprises the brain and spinal cord. In MS, the immune system mistakenly attacks the protective covering of nerve fibers, known as myelin, resulting in inflammation and damage. This damage disrupts the normal flow of electrical impulses along the nerves, leading to a wide range of symptoms that vary from person to person.
Types of Multiple Sclerosis
Multiple sclerosis can manifest in various forms, each with its unique characteristics and progression patterns. Understanding these different types can help patients and their healthcare providers develop the most effective treatment plans. The main types of MS include:
Radiologically Isolated Syndrome (RIS): RIS is characterized by the presence of lesions in the central nervous system, as seen on MRI scans, without any clinical symptoms. People with RIS have a higher risk of developing MS, but not all will progress to the symptomatic stages.
Clinically Isolated Syndrome (CIS): CIS refers to a single episode of neurological symptoms lasting at least 24 hours, caused by inflammation or demyelination in the CNS. While CIS may be an early sign of MS, not everyone with CIS will go on to develop the condition.
Relapsing-Remitting MS (RRMS): RRMS is the most common form of MS, affecting approximately 85% of those diagnosed. Patients with RRMS experience clearly defined relapses of worsening symptoms, followed by periods of partial or complete recovery (remission). The disease course in RRMS is highly variable and unpredictable. RRMS is the most common initial form of MS. Younger patients are more likely to have this form of MS than older patients.
Secondary Progressive MS (SPMS): SPMS is a stage that can develop after years of living with RRMS. In SPMS, patients experience a gradual worsening of symptoms over time, with or without relapses. Disability tends to progress more steadily in this stage.
Primary Progressive MS (PPMS): PPMS affects about 10-15% of people with MS and is characterized by a gradual worsening of symptoms from the onset, without distinct relapses or remissions. The rate of progression can vary, but PPMS generally leads to more severe disability earlier in the disease course compared to other forms of MS.
Causes and Risk Factors for MS
The exact cause of MS remains unknown, but it is believed to involve a combination of genetic and environmental factors. Some possible risk factors include:
Age: MS typically occurs between the ages of 20 and 50.
Gender: Women are about two to three times more likely to develop MS than men.
Family history: Having a close family member with MS increases your risk.
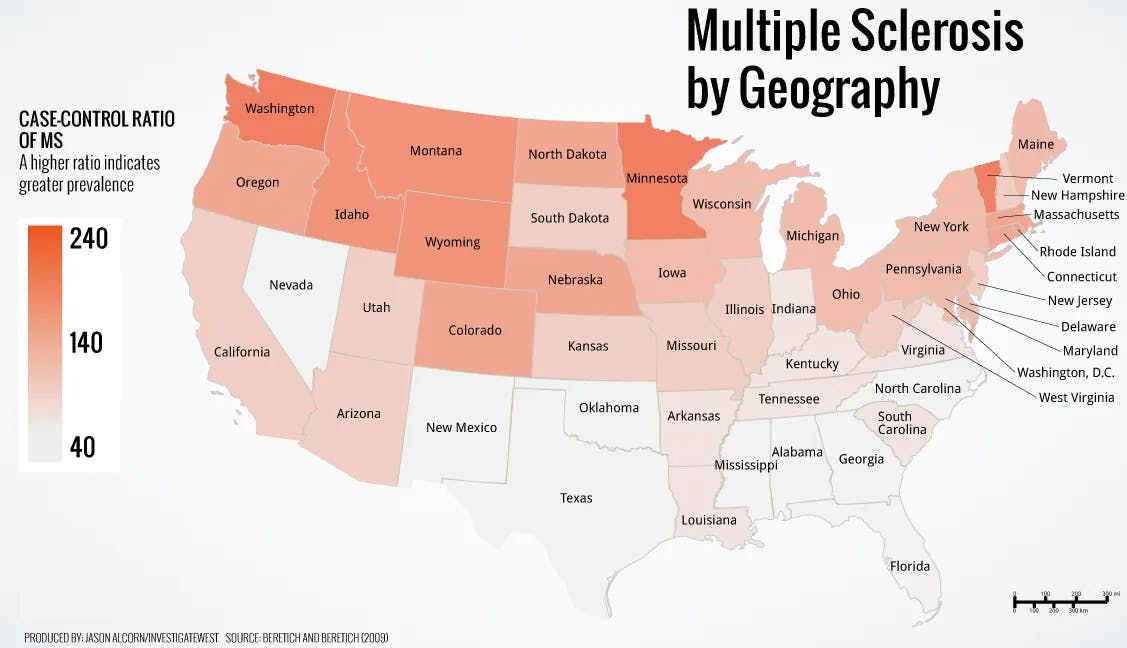
Geography: MS is more common in countries further from the equator.
Infections: Some viral infections, such as the Epstein-Barr virus, have been linked to MS.
Smoking: Cigarette smoking has been found to increase the risk of developing MS and may also contribute to a more severe disease course. Quitting smoking can not only reduce the risk of MS but also provide numerous other health benefits.
Obesity: Studies have shown that obesity, particularly during adolescence, can increase the risk of developing MS. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce this risk.
Vitamin D deficiency: Low levels of vitamin D have been associated with a higher risk of MS. The exact role of vitamin D in MS development remains unclear, but it is thought to play a role in immune system function. Ensuring adequate vitamin D intake through diet, supplementation, or sensible sun exposure can help reduce the risk of MS.
Common MS Symptoms
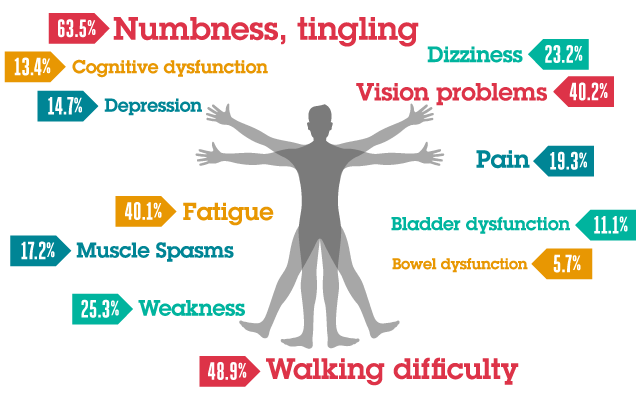
The symptoms of MS can vary widely from person to person, as they depend on the location and extent of the nerve damage. Some common symptoms include:
Fatigue: Fatigue in MS can be overwhelming and persistent, making it difficult to complete daily tasks or engage in activities. It can also be exacerbated by heat, stress, or physical exertion.
Numbness or tingling in limbs: These sensations, often described as 'pins and needles' or a loss of sensation, are typically among the first symptoms experienced by individuals with MS and can occur in the hands, feet, arms, or legs.
Muscle weakness or stiffness: People with MS may experience muscle weakness, which can lead to difficulty walking or performing daily activities, and stiffness, which can cause discomfort and limit the range of motion.
Vision problems: MS can cause optic neuritis, inflammation of the optic nerve, resulting in blurred vision, loss of color vision, or even temporary vision loss in one eye. It can also cause double vision, which can be a sign of inflammation in the back of the brain.
Dizziness and balance issues: Individuals with MS may experience dizziness or vertigo, giving them a sensation of spinning or unsteadiness, which can contribute to difficulty with coordination and balance.
Bladder and bowel dysfunction: MS can affect the nerves controlling bladder and bowel function, leading to issues such as frequent or urgent urination, incontinence, constipation, or loss of bowel control.
Cognitive difficulties: People with MS may experience cognitive challenges, such as difficulty with memory, concentration, information processing, or problem-solving, which can impact daily life and work.
Emotional changes: MS can cause emotional changes, such as depression, mood swings, or irritability, which may be a result of the disease's impact on the brain or a reaction to the challenges of living with MS.
MS Diagnosis

Diagnosing multiple sclerosis can be a complex and sometimes lengthy process, as there is no single definitive test for the condition. Instead, healthcare professionals rely on a combination of methods to determine if a patient has MS. Early diagnosis and treatment are crucial for managing symptoms and potentially slowing the progression of the disease. The diagnostic process typically involves the following steps:
Medical history and physical examination: A neurologist will review the patient's medical history and conduct a thorough physical examination, focusing on assessing the nervous system. This helps identify any patterns or symptoms that may suggest MS.
Magnetic Resonance Imaging (MRI): MRI scans are instrumental in diagnosing MS, as they can reveal areas of damage or inflammation in the brain and spinal cord. These scans can also help rule out other conditions with similar symptoms.
Additional tests: Depending on the patient's specific symptoms and medical history, other tests may be conducted to support the diagnosis. These tests can include a lumbar puncture (spinal tap) to analyze cerebrospinal fluid for signs of inflammation, and Optical Coherence Tomography (OCT) to assess the thickness of the retinal nerve fiber layer in the eyes, which can be an indirect indicator of nerve damage in the central nervous system.
Diagnostic criteria: To confirm a diagnosis of MS, a neurologist will use the McDonald Criteria, which is a set of guidelines that require evidence of damage in at least two separate areas of the central nervous system, occurring at different points in time, and with no other explanation for the symptoms.
MS Treatments

The management of multiple sclerosis involves a combination of treatments aimed at modifying the disease course, managing symptoms, and addressing relapses. Early and aggressive intervention is crucial for preventing future disability and maintaining a better quality of life. It's crucial for patients and healthcare providers to collaborate closely and develop a personalized treatment plan to manage the condition effectively.
Disease-modifying therapies (DMTs): DMTs are medications designed to reduce the frequency and severity of relapses, slow down the progression of the disease, and decrease the accumulation of lesions in the CNS. There are various DMTs available, including injectable, oral, and infusion therapies. Early and aggressive treatment with DMTs is essential for limiting long-term disability and improving overall prognosis.
Symptom management: MS can present with a wide range of symptoms, and tailored treatments are required to address each person's unique needs. This may involve medications for fatigue, muscle stiffness, pain, and bladder or bowel dysfunction, as well as physical therapy, occupational therapy, and speech therapy to improve mobility, strength, and daily function.
Treatment of relapses: In the event of a relapse, patients may require short-term treatments such as corticosteroids to reduce inflammation and hasten recovery. In more severe cases, other therapies such as plasmapheresis may be considered.
Lifestyle and support: A comprehensive approach to MS treatment should also include lifestyle modifications and support services. Regular exercise, a balanced diet, stress reduction techniques, and adequate sleep are essential for overall well-being. Patients should also consider joining support groups and seeking counseling to help navigate the emotional challenges associated with living with MS.
Frequently Asked Questions
How do you know if you have MS?
Diagnosing MS can be challenging, as there is no single test that can definitively identify the condition. Instead, neurologists rely on a combination of medical history, neurological exams, and imaging tests such as MRI to make a diagnosis. If you suspect you may have MS, it's important to consult a healthcare professional for a thorough evaluation.
Can men get MS?
Yes, men can get MS, although women are about two to three times more likely to develop the condition. The reasons for this gender disparity are not yet fully understood.
Can you have MS without knowing?
It is possible to have MS without knowing, as the early symptoms can be mild and may not cause significant disruption to daily life. Additionally, MS symptoms can be similar to those of other conditions, leading to misdiagnosis or delayed diagnosis. However, as the disease progresses, symptoms typically become more pronounced, leading individuals to seek medical attention.
Can you have MS without numbness?
Yes, it is possible to have MS without experiencing numbness. MS symptoms vary widely from person to person, and not everyone with the condition will experience the same set of symptoms. While numbness or tingling in the limbs is a common symptom, other individuals may initially experience different symptoms, such as fatigue, vision problems, or muscle weakness.
Can you get MS in your 20s, 30s, or 50s?
MS can affect people at any age but is most commonly diagnosed between the ages of 20 and 50. However, it's possible to develop MS outside of this age range.
How do I get diagnosed with MS?
If you suspect you may have MS, consult a healthcare professional, preferably a neurologist. They will take your medical history, perform a neurological examination, and may order additional tests such as an MRI, spinal tap, or evoked potentials to help confirm a diagnosis.
Can you have MS with a normal MRI?
While MRI is a crucial tool in diagnosing MS, it is possible, though rare, to have MS with a normal or inconclusive MRI. In such cases, other diagnostic tests, such as spinal taps or evoked potentials, may provide additional information to help confirm a diagnosis.
Can you have MS symptoms without having MS?
Some MS symptoms, such as fatigue, numbness, or muscle weakness, can also be caused by other conditions. If you experience symptoms that resemble MS, it's important to consult a healthcare professional for a thorough evaluation to determine the underlying cause.
Do MS symptoms get worse throughout the day?
MS symptoms can fluctuate throughout the day and may be influenced by factors such as fatigue, stress, or heat. Some people with MS may find that their symptoms worsen as the day progresses, especially if they are experiencing fatigue or have been physically active. However, symptom patterns can vary greatly between individuals, and not everyone will experience worsening symptoms throughout the day.
Do MS symptoms get worse when tired?
Yes, fatigue can exacerbate MS symptoms, making them feel worse or more difficult to manage. Fatigue is a common symptom of MS and can significantly impact an individual's daily functioning. It is essential for people with MS to manage their energy levels, prioritize rest, and develop strategies to cope with fatigue.
Do steroids help MS?
Steroids, specifically corticosteroids, can be used to help manage MS relapses. They work by reducing inflammation and suppressing the immune system's overactivity, which can help alleviate MS symptoms and shorten the duration of a relapse. Steroids are typically used as a short-term treatment during acute episodes and are not a long-term solution for managing MS.
Do women get MS?
Yes, women can develop MS, and they are, in fact, two to three times more likely to have the condition than men. The reasons for this gender disparity are not yet fully understood, but it is believed that hormonal and genetic factors may contribute to this difference.
Do you have memory loss with MS?
Memory loss and cognitive difficulties can be a symptom of MS, affecting up to 50% of people with the condition. These cognitive issues may include problems with memory, concentration, information processing, and problem-solving. The severity of cognitive symptoms varies from person to person and can have a significant impact on daily functioning and quality of life.
Can you get MS from an injury?
There is no evidence to suggest that MS can be caused by a physical injury. MS is believed to result from a combination of genetic and environmental factors, such as viral infections or low levels of vitamin D.
Can you get vaccinated if you have MS?
People with MS can generally receive vaccinations, but it's important to discuss your specific situation with your healthcare provider. Some vaccines may not be recommended for individuals taking certain disease-modifying therapies, while others may be particularly important for people with MS to help prevent infections that could worsen their condition.
Do MS symptoms get worse when tired?
Fatigue is a common symptom of MS and can exacerbate other symptoms, such as cognitive difficulties, muscle weakness, or balance problems. It's essential for people with MS to manage their energy levels, prioritize rest, and develop strategies to cope with fatigue.
What to do if you think you have MS?
If you suspect you may have MS, it's crucial to consult a healthcare professional, such as your primary care doctor or a neurologist. They will help evaluate your symptoms, perform the necessary tests, and, if needed, develop an appropriate treatment plan. Early diagnosis and intervention can significantly impact the course of the disease and improve the quality of life for people with MS.
What are the long-term effects of MS?
The long-term effects of MS can vary widely and depend on the individual and the severity of their disease. Some individuals may experience worsening disability over time, while others may only have mild symptoms. In general, MS can lead to a decrease in mobility, difficulty with daily activities, and an increased risk of depression and other mental health issues. It is important to work closely with your healthcare provider to manage your MS and prevent long-term complications by starting treatment early.
What is the prognosis for individuals with MS?
The prognosis for individuals with MS can vary widely and depends on several factors, such as the severity of the disease, the individual's age, and how well the disease is managed. In general, most individuals with MS can expect to live a normal life if they start an effective treatment early in their disease course.
What are the risk factors for developing MS?
The exact cause of RRMS is unknown, but certain factors may increase an individual's risk of developing the disease. These include:
Age: MS is most commonly diagnosed in individuals between the ages of 20 and 40.
Gender: MS is more common in women than men.
Family history: Individuals with a family history of MS may have a slightly increased risk of developing the disease.
Environmental factors: Exposure to certain environmental factors, such as Epstein-Barr Virus, low levels of vitamin D, or smoking may increase an individual's risk of developing MS.
What are the available support resources for individuals with MS?
There are many support resources available for individuals with MS, including support groups, online forums, and informational websites. Additionally, healthcare providers and social workers can provide support and guidance on managing the disease and coping with its effects. Please go to the resources section of our website for more information.
Can MS be cured?
Currently, there is no cure for MS. However, early diagnosis and treatment can help manage the symptoms, prevent disability and slow the progression of the disease. While there is no cure for MS, ongoing research is being conducted to better understand the disease and develop new treatments that may be able to halt or reverse its effects. In the meantime, individuals with MS can work with their healthcare team to manage their symptoms and maintain a good quality of life
How do I find out if I have MS?
If you suspect you may have MS, it is crucial to consult a healthcare professional, specifically an MS specialist neurologist. They will help evaluate your symptoms, perform the necessary tests, and, if needed, develop an appropriate treatment plan. Early diagnosis and intervention can significantly impact the course of the disease and improve the quality of life for people with MS.
How does someone get multiple sclerosis?
The exact cause of MS is not yet fully understood, but it is believed to be a result of a combination of genetic and environmental factors. Some possible factors include a predisposition due to genetic makeup, viral infections, low levels of vitamin D, and certain lifestyle factors such as smoking and obesity. MS is an autoimmune disease, where the immune system mistakenly attacks the protective covering of nerve fibers called myelin, leading to inflammation and nerve damage.
What should I do if I think I have MS?
If you think you may have MS, it's important to consult a healthcare professional, preferably a neurologist specializing in MS. They will take your medical history, perform a neurological examination, and may order additional tests such as an MRI, blood tests or spinal tap to help confirm a diagnosis. Early diagnosis and intervention can improve the long-term prognosis and help manage symptoms more effectively. It's also important to educate yourself about the condition and connect with support networks to help you navigate the challenges of living with MS.
Experience Comprehensive MS Care at our Beverly Hills MS Clinic
Our experienced team at the Beverly Hills MS Clinic offers advanced telehealth services for patients with MS, providing personalized care and support to manage symptoms and improve quality of life. Book an appointment with us today and take the first step towards managing your MS.